Attention Deficit Disorder (ADD) is a neurodevelopmental condition characterized by persistent inattention, hyperactivity, and impulsivity, affecting both children and adults. It is marked by difficulties in maintaining focus and regulating behavior, often impacting daily functioning and quality of life. Early recognition and appropriate management are crucial for improving outcomes and reducing long-term consequences.
1.1 Definition and Overview
Attention Deficit Disorder (ADD) is a neurodevelopmental condition characterized by persistent patterns of inattention, hyperactivity, and impulsivity. It is now classified under Attention-Deficit/Hyperactivity Disorder (ADHD) in the DSM-5, which recognizes three presentations: predominantly inattentive, predominantly hyperactive-impulsive, and combined. ADD/ADHD affects both children and adults, impacting daily functioning, academic performance, and social interactions. It is marked by difficulties in sustaining focus, following instructions, and controlling impulses, often leading to challenges in maintaining relationships and achieving personal goals.
1.2 Historical Context and Evolution of Understanding
Attention Deficit Disorder (ADD) has evolved significantly in its conceptualization. Historically, symptoms of inattention and hyperactivity were first recognized in the early 20th century. The DSM-III (1980) introduced ADD as a distinct diagnosis, distinguishing it from hyperactivity. Subsequent editions, including DSM-IV and DSM-5, refined criteria, incorporating ADHD as an umbrella term. Early understanding often linked it to “minimal brain dysfunction,” but modern perspectives emphasize neurodevelopmental origins, acknowledging the condition’s complexity and variability across ages.
1.3 Importance of Early Diagnosis and Treatment
Early diagnosis and intervention are critical for managing Attention Deficit Disorder (ADD). Untreated ADHD can lead to academic underachievement, social challenges, and emotional difficulties. Timely identification allows for targeted strategies to reduce symptoms and improve functioning. Delayed diagnosis often results in prolonged struggles, affecting self-esteem and relationships. Effective treatments, such as medications and behavioral therapies, can significantly enhance quality of life when implemented early, emphasizing the need for prompt and accurate assessment.

Diagnostic Criteria for ADHD
ADHD is characterized by persistent symptoms of inattention, hyperactivity, and impulsivity, lasting at least six months, present in multiple settings, and impacting functioning.
2.1 DSM-5 Criteria for ADHD
The DSM-5 requires at least five symptoms of inattention and/or hyperactivity-impulsivity to be present for six months, with onset before age 12. Symptoms must cause significant impairment in two or more settings, such as home, school, or work. The DSM-5 also introduced changes, including the recognition of ADHD in adults and the addition of severity specifiers. These criteria help clinicians accurately diagnose and differentiate ADHD from other conditions, ensuring appropriate treatment plans.
2.2 Differences Between ADD and ADHD
Attention Deficit Disorder (ADD) is an outdated term for what is now referred to as Attention-Deficit/Hyperactivity Disorder (ADHD), predominantly inattentive type. While both involve difficulties with focus, ADHD includes hyperactivity and impulsivity. ADD historically described individuals with inattention without hyperactivity. The DSM-5 unified these into ADHD with different presentations. Despite the change, “ADD” is still informally used to describe inattentive symptoms without hyperactivity, though it is no longer an official diagnosis.
2.3 DSM-IV vs. DSM-5: Key Changes
The DSM-5 introduced significant updates to ADHD criteria. It raised the symptom threshold for adults from 6 to 5, allowed for a broader age of onset (up to 12 years), and combined subtypes into three presentations. The DSM-5 also acknowledged ADHD as a valid adult diagnosis and added a “other specified” and “unspecified” category for borderline cases. These changes aim to improve diagnostic accuracy and accommodate the disorder’s complexity across the lifespan.
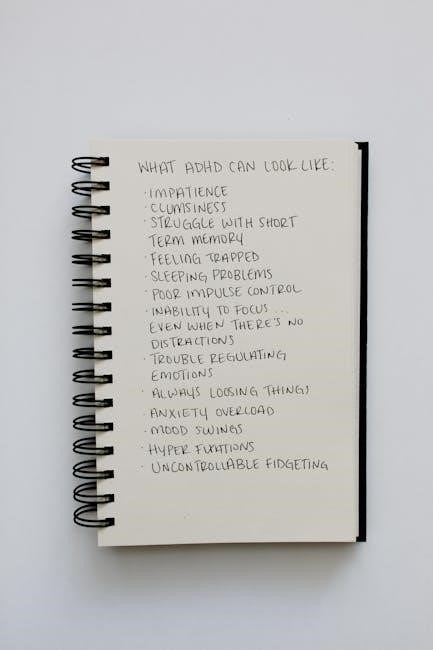
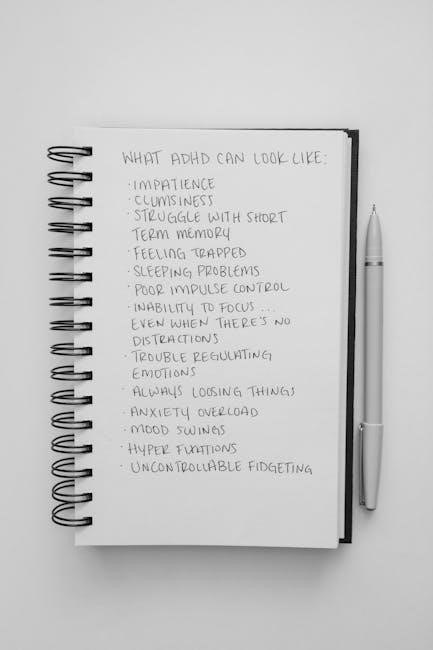
Symptoms of Attention Deficit Disorder
Attention Deficit Disorder is marked by persistent inattention, hyperactivity, and impulsivity, impacting daily functioning and relationships. Symptoms vary but often include difficulty focusing and regulating behavior.
3.1 Inattention Symptoms
Inattention symptoms of Attention Deficit Disorder include difficulty sustaining focus, following detailed instructions, and completing tasks. Individuals often appear distractible, struggling to stay engaged in activities. They may frequently lose items, forget responsibilities, or make careless mistakes. These symptoms disrupt daily functioning and learning, as affected individuals may seem disorganized or forgetful, failing to meet expectations at work or school. Such challenges are central to the disorder’s impact on productivity and relationships.
3.2 Hyperactivity Symptoms
Hyperactivity symptoms of Attention Deficit Disorder involve excessive physical activity, restlessness, and an inability to stay still. Individuals may exhibit fidgeting, tapping, or trouble remaining seated in quiet environments. They often feel compelled to move, even when inappropriate, and may talk excessively or interrupt others. These behaviors can disrupt social interactions and daily activities, particularly in structured settings like classrooms or workplaces. Hyperactivity can vary in severity but often persists across different environments, affecting overall functioning and relationships.
3.3 Impulsivity Symptoms
Impulsivity symptoms of Attention Deficit Disorder involve acting without considering consequences, interrupting others, and difficulty waiting turns. Individuals may blurt out answers prematurely or engage in risky behaviors. Impulsive actions often disrupt social interactions and daily tasks, leading to interpersonal challenges. These behaviors stem from poor self-control and difficulty regulating impulses, which can result in unintended outcomes. Impulsivity can manifest differently across ages, but it consistently interferes with functioning and relationships, requiring targeted strategies for management and improvement.
Prevalence and Demographics
Attention Deficit Disorder affects 5-8% of children, primarily boys, and often persists into adulthood, impacting daily functioning and quality of life globally.
4.1 ADHD in Children vs. Adults
Attention Deficit Hyperactivity Disorder (ADHD) is most commonly diagnosed in children, with symptoms often persisting into adulthood. In children, ADHD typically presents as inattention, hyperactivity, and impulsivity, disrupting academic and social functioning. Adults with ADHD may experience more subtle symptoms, such as difficulties with time management, organization, and emotional regulation. While children are more likely to exhibit overt hyperactivity, adults often struggle with inner restlessness and persistent distractibility, highlighting the evolutionary nature of symptoms across the lifespan.
4.2 Gender Differences in Diagnosis
Attention Deficit Hyperactivity Disorder (ADHD) is more commonly diagnosed in males than females, with a significant gender disparity in recognition and treatment. Boys are often diagnosed in childhood due to overt hyperactivity, while girls may go undiagnosed until adulthood, as they are more likely to exhibit inattentive symptoms. This disparity stems from differing symptom presentations and societal expectations, highlighting the need for improved awareness and diagnostic tools to address ADHD equally across genders and ensure timely intervention for all individuals.
4;3 Global Prevalence Rates
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most common neurodevelopmental disorders worldwide, with a global prevalence of approximately 5-8% in children and 2-5% in adults. According to the DSM-5, ADHD affects individuals across diverse regions, with higher rates observed in North America compared to Europe and Asia. Regional differences in diagnostic practices, cultural perceptions, and awareness contribute to variations in reported prevalence, emphasizing the need for standardized diagnostic criteria and increased global awareness to ensure accurate identification and support for affected individuals.

Causes and Risk Factors
Attention Deficit Disorder (ADD) stems from a combination of genetic, environmental, and neurobiological factors, including brain structure differences and prenatal exposures, influencing its development and severity.
5.1 Genetic Factors
Genetic factors significantly contribute to Attention Deficit Disorder (ADD), with heritability estimates suggesting 70-90% of the risk is inherited. Specific genes, such as DRD4 and DAT1, are linked to dopamine regulation, impacting attention and behavior. Family studies reveal a higher prevalence among first-degree relatives of individuals with ADD, highlighting a strong familial component.
These genetic predispositions often interact with environmental factors, influencing the development and severity of symptoms. Understanding the genetic basis helps in early identification and tailored interventions.
5.2 Environmental Influences
Environmental factors play a significant role in the development and severity of Attention Deficit Disorder (ADD). Prenatal exposure to substances like tobacco and alcohol, as well as maternal stress during pregnancy, have been linked to an increased risk. Postnatal influences, such as family dynamics, parenting styles, and socioeconomic status, also contribute. Additionally, environmental toxins and dietary factors may exacerbate symptoms in genetically predisposed individuals.
These external factors often interact with genetic predispositions, shaping the manifestation of ADD. Understanding these influences is crucial for developing targeted interventions and lifestyle modifications to manage symptoms effectively.
5.3 Neurobiological Aspects
Attention Deficit Disorder (ADD) is associated with distinct neurobiological features, including differences in brain structure and function. Key regions, such as the prefrontal cortex, exhibit altered activity, impacting executive functioning. Imbalances in neurotransmitters like dopamine and norepinephrine are also observed, affecting attention and impulse control. Neuroimaging studies highlight variations in neural connectivity and cortical thickness in individuals with ADD, providing insights into its biological underpinnings. These findings underscore the complex interplay between brain chemistry and behavior in the disorder.
Comorbid Conditions
Individuals with Attention Deficit Disorder often experience co-occurring mental health issues, such as depression, anxiety, or behavioral disorders, complicating diagnosis and treatment approaches.
6.1 Co-occurring Mental Health Disorders
Attention Deficit Disorder often co-occurs with other mental health conditions, such as depression, anxiety, or mood disorders, which can complicate diagnosis and treatment. These comorbidities require comprehensive diagnostic evaluations to ensure accurate identification and management. Integrated treatment plans addressing both ADHD and co-occurring disorders are essential for optimal outcomes. Mood disorders, anxiety, and learning disabilities are common among individuals with ADHD, highlighting the need for a holistic approach to care.
6.2 Impact on Daily Life and Functioning
Attention Deficit Disorder significantly impacts daily life, affecting academic, professional, and social functioning. Individuals often struggle with maintaining focus, completing tasks, and managing time effectively. This can lead to challenges in relationships, educational underachievement, and workplace difficulties. Persistent symptoms of inattention, hyperactivity, and impulsivity can disrupt routines and overall quality of life. Early intervention and tailored strategies are essential to mitigate these challenges and improve functional outcomes across various life domains.
6.3 Differential Diagnosis
Differential diagnosis is critical to ensure accurate identification of Attention Deficit Disorder, as symptoms can overlap with other conditions like anxiety, mood disorders, or sleep disturbances. Clinicians must rule out alternative diagnoses by conducting thorough evaluations, including clinical interviews and behavioral assessments. Co-occurring disorders are common, and proper differentiation is essential for effective treatment planning. Specialist input and standardized tools help confirm the diagnosis and distinguish it from other mental health conditions with similar presentations.

Diagnosis and Assessment
Diagnosis involves a comprehensive clinical evaluation using DSM-5 criteria, including detailed patient history, behavioral observations, and standardized assessment tools to confirm symptoms and rule out other conditions.
7.1 Clinical Evaluation Process
The clinical evaluation for Attention Deficit Disorder involves a comprehensive assessment using DSM-5 criteria, including a detailed patient history, behavioral observations, and symptom rating scales. Specialists such as psychiatrists or psychologists conduct interviews with patients and their families to assess symptom severity, duration, and impact on daily life. This process helps differentiate ADHD from other conditions, ensuring an accurate diagnosis and appropriate treatment plan.
7.2 Screening Tools and Scales
Common screening tools for ADHD include the Conners’ Rating Scales, Vanderbilt Assessment Scale, and ADHD Rating Scale-IV. These tools assess symptoms of inattention, hyperactivity, and impulsivity across home and school settings. Clinicians use standardized questionnaires completed by parents, teachers, and patients to evaluate symptom severity. These scales help identify potential ADHD cases and differentiate them from other conditions, ensuring accurate diagnosis and appropriate intervention planning.
7.3 Role of Specialists in Diagnosis
Specialists such as psychiatrists, psychologists, and pediatricians play a crucial role in diagnosing ADHD. They conduct comprehensive clinical evaluations, utilizing DSM-5 criteria and screening tools to assess symptoms. Collaboration with teachers and parents provides a holistic view of the individual’s behavior. Specialists also rule out comorbid conditions and develop personalized treatment plans. Their expertise ensures accurate diagnosis and effective management, addressing the unique needs of each patient to improve overall functioning and quality of life.
Treatment and Management
Treatment for ADHD often involves a combination of medications, behavioral therapies, and lifestyle modifications. Medications are typically the first line of treatment, helping to manage symptoms effectively.
8.1 Medications for ADHD
Medications for ADHD, primarily stimulants and non-stimulants, help regulate brain chemistry to improve focus and reduce hyperactivity. Stimulants, like methylphenidate and amphetamines, are most commonly prescribed. Non-stimulant options, such as atomoxetine, are alternatives for those who cannot take stimulants. These medications aim to enhance dopamine and norepinephrine levels, improving attention and impulse control. Dosage and type are tailored to individual needs, requiring regular monitoring by healthcare providers to ensure effectiveness and minimize side effects.
8.2 Behavioral Therapies and Interventions
Behavioral therapies are evidence-based interventions for ADHD, focusing on improving skills and reducing symptoms. Techniques like cognitive-behavioral therapy (CBT), positive reinforcement, and organizational training help individuals manage inattention and impulsivity. These interventions often involve creating structured routines, setting clear goals, and using token systems to encourage positive behavior. Behavioral therapy is typically used alongside medication and is tailored to the individual’s needs, providing tools for better emotional regulation and daily functioning.
8.3 Lifestyle and Environmental Modifications
Lifestyle and environmental changes play a crucial role in managing ADHD symptoms. Creating a structured and predictable environment helps reduce chaos, while consistent routines improve time management and organization. Regular physical activity, especially outdoors, has been shown to enhance focus and reduce hyperactivity. A balanced diet, adequate sleep, and stress reduction techniques like mindfulness can also positively impact symptoms. These modifications, when tailored to individual needs, can significantly improve daily functioning and overall well-being for those with ADHD.

Coping Strategies and Support Systems
Effective coping strategies include structured routines, organizational tools, and mindfulness practices. Support from family, peers, and support groups can significantly improve daily functioning and emotional well-being.
9.1 Educational Accommodations
Educational accommodations for individuals with ADHD include tailored learning plans, extended test time, and the use of assistive technology. These strategies help students stay organized and focused, ensuring equal access to education. Schools often develop Individualized Education Programs (IEPs) or 504 plans to address specific needs. These accommodations aim to enhance academic performance and overall educational experiences, providing necessary support to help individuals with ADHD thrive in learning environments.
9.2 Family and Peer Support
Family and peer support play a vital role in managing ADHD. Families can create structured environments, offer emotional encouragement, and help with organization. Peers can provide understanding and inclusion, reducing stigma. Open communication and education about ADHD foster empathy and support. Resources like books (e.g., “Driven to Distraction” by Hallowell and Ratey) and organizations (e.g., CHADD) offer guidance for families and peers, promoting a supportive network for individuals with ADHD.
9.3 Self-Help Resources and Books
Self-help resources and books provide valuable strategies for managing ADHD. Titles like “You Mean I’m Not Lazy, Stupid or Crazy?” by Hallowell and Ratey, and “Driven to Distraction” offer practical advice and emotional support. These resources help individuals and families understand ADHD, develop coping mechanisms, and improve daily functioning. Online communities and apps also serve as tools for tracking progress and staying motivated, empowering individuals to take control of their condition effectively.

Specialized Resources and Guidelines
The National Resource Center on ADHD and CHADD provide evidence-based guidelines, while CDC recommendations ensure accurate diagnosis and treatment. These resources aid in managing ADHD effectively.
10.1 National Resource Center on ADHD
The National Resource Center on ADHD, operated by CHADD, provides comprehensive resources and support for individuals with ADHD and their families. It offers a helpline (1-800-233-4050) staffed by trained professionals to address questions and concerns. The center’s website features links to educational materials, treatment guidelines, and community connections. These resources aim to enhance understanding, improve care, and empower those affected by ADHD to manage their condition effectively and lead fulfilling lives.
10.2 CDC and CHADD Recommendations
The CDC and CHADD provide guidelines for ADHD management, emphasizing early diagnosis and evidence-based treatments. The CDC recommends comprehensive assessments and individualized care plans. CHADD’s National Resource Center offers educational materials, helpline support, and advocacy programs. These recommendations aim to improve ADHD care, ensuring access to accurate information and effective interventions for individuals and families. Their collaborative efforts promote awareness and support, fostering better outcomes for those affected by ADHD.
10.3 Evidence-Based Practice Guidelines
Evidence-based practice guidelines for ADHD emphasize comprehensive diagnostic assessments and individualized treatment plans. The American Academy of Pediatrics recommends behavioral therapy as a first-line treatment for children, alongside medication for severe cases. The National Institute for Health and Care Excellence (NICE) suggests a multimodal approach, including psychoeducation and lifestyle adjustments. Regular monitoring and adjustments to treatment are crucial to ensure effectiveness and minimize side effects, promoting long-term management of ADHD symptoms and improving quality of life.

Emerging Research and Trends
Emerging research focuses on telehealth advancements, digital monitoring tools, and global perspectives to enhance ADHD diagnosis and management, improving accessibility and care standardization worldwide.
11.1 Advances in Neuroimaging
Recent advancements in neuroimaging, such as functional MRI (fMRI) and magnetic resonance imaging (MRI), have significantly enhanced the understanding of brain structure and function in individuals with ADHD. These technologies allow researchers to identify differences in brain activity and connectivity, particularly in regions related to attention and impulse control. Neuroimaging has also facilitated early diagnosis and monitoring of treatment responses, providing valuable insights into the neurobiological underpinnings of the disorder. Such innovations are paving the way for more personalized and effective interventions.
11.2 Telehealth and Digital Tools
Telehealth and digital tools have revolutionized ADHD care, enhancing accessibility and convenience. Remote consultations and online platforms now enable individuals to receive diagnoses and support from specialists worldwide. Mobile apps and digital trackers help monitor symptoms, improve organization, and provide therapeutic interventions. These innovations are particularly beneficial for adults and children with ADHD, offering flexible solutions to manage symptoms and improve daily functioning, reducing stigma and increasing early intervention opportunities.
11.3 Global Perspectives on ADHD
Attention Deficit Hyperactivity Disorder (ADHD) is recognized globally, with varying prevalence rates and cultural perceptions. In Europe, the International Classification of Diseases (ICD) is often used alongside the DSM-5. Cultural differences influence diagnosis and treatment approaches, with some regions emphasizing behavioral therapies over medication. Global collaborations and awareness campaigns aim to standardize care and reduce stigma, ensuring equitable access to ADHD management worldwide, fostering a more inclusive understanding of neurodevelopmental disorders.
Attention Deficit Disorder is a complex condition requiring comprehensive care. Early diagnosis, tailored treatments, and ongoing support are essential for improving quality of life and outcomes.
12.1 Summary of Key Points
Attention Deficit Disorder (ADD) is a neurodevelopmental condition marked by symptoms of inattention, hyperactivity, and impulsivity. It affects both children and adults, impacting daily functioning and quality of life. Early diagnosis and tailored interventions are critical for managing symptoms and improving outcomes. The disorder is influenced by genetic, environmental, and neurobiological factors, and its diagnosis involves clinical evaluations and standardized criteria. Treatment often combines medications, behavioral therapies, and lifestyle adjustments to address challenges and enhance overall well-being. Raising awareness and providing support systems are essential for individuals with ADD to thrive.
12.2 Future Directions in ADHD Care
Future directions in ADHD care emphasize personalized medicine, leveraging genetic insights and advanced neuroimaging to tailor treatments. Telehealth and digital tools are expanding access to care, especially for underserved populations. Research into non-invasive neurotechnologies, such as brain stimulation, offers promising alternatives. Enhancing early intervention programs and addressing health disparities are priorities. Global collaborations aim to standardize care and improve outcomes, ensuring equitable access to evidence-based therapies for individuals with ADHD worldwide.
12.3 Call to Action for Awareness
Raising awareness about ADHD is crucial for reducing stigma and ensuring early diagnosis. Educating the public, educators, and healthcare providers about ADHD symptoms and treatments can improve understanding and support. Advocating for accessible resources and inclusive policies fosters equitable care. Encourage open conversations to promote acceptance and empower individuals with ADHD to thrive. Share reliable information and support research to advance care and awareness globally.
